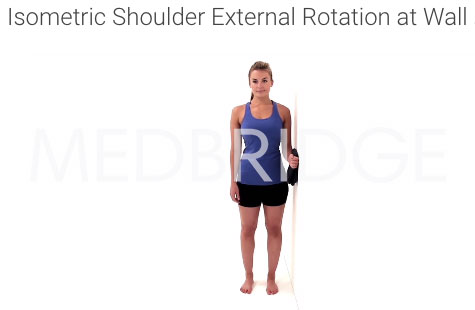
The wall isometric isn't as "functional" as the reactive or stepping isometric, but does that make it worse? I used to prescribe the stepping isometric to every shoulder patient, that wasn't ready for isotonics, but now I only occasionally do. Why? Barriers to adherence limit this exercise:
It requires equipment that you have to provide or the patient has to buy
The equipment must be set up each time and available
If the elbow is tucked too tightly to the side of the body, load through the shoulder is mitigated
Steeper learning curve and reduced self efficacy (3)
Now I go with the standard isometric. The only equipment needed for adherence is a wall, and let's face it, most people a one "lying around"...
I never thought I'd be thinking about my eccentric, freshman biology teacher on a daily basis... Keep It Simple Stupid
References
1. Henry, Kristin D., Cherie Rosemond, and Lynn B. Eckert. "Effect of number of home exercises on compliance and performance in adults over 65 years of age." Physical Therapy 79.3 (1999): 270-277.
2. Littlewood, Chris, et al. "A self-managed single exercise programme versus usual physiotherapy treatment for rotator cuff tendinopathy: A randomised controlled trial (the SELF study)."Clinical rehabilitation (2015): 0269215515593784.
3. McLean, Sionnadh Mairi, et al. "Interventions for enhancing adherence with physiotherapy: a systematic review." Manual therapy 15.6 (2010): 514-521.
4. Der Ananian, Cheryl, et al. "Factors associated with exercise participation in adults with arthritis." J Aging Phys Act 16.2 (2008): 125-143.
Images:
Flickr Via Ben Russel "Teacher"
Thank you MedBridge for permitting use of the isometric images.
** This information is not intended to replace the advice of a physician/ physical therapist. Andy Parsons, PT, DPT disclaims any liability for the decisions you make based on this information.