By Andy Parsons, PT, DPT
Over the last year, I have been thinking critically about how I prescribe exercises in the clinic. As a new grad, I focused on making exercise prescription unique and functional. After all, the PT profession did go through the "functional exercise" revolution around the new millennium. You know, each exercise that we prescribe must mimic that functional activity that our client needs to perform to get back to full function. Well, maybe... that is, if the exercise doesn't get too elaborate for it's own good.
After all, Isn't the best exercise the one that get's done?
I'm not throwing function completely out the window, but I now balance that thought with another main principle - the KISS method
KISS: Keep It Simple Stupid.
Yep, Keep It Simple Stupid. The "scientific" saying first introduced to me by my high school freshmen biology teacher. Okay, seriously though, my rationale is based in some science. We do know HEP performance quality is improved with 2 exercises prescribed 8 (1). Meaning increased exercise number likely decreases quality of exercise performed. I'm also reminded of a recent study that indicated one simple abduction exercise was as effective for RTC tendinopathy as "standard care" (2). Also, if your "functional exercise" is still taking multiple verbal cues and tactile cues for quality after a few sessions, it is NOT getting done right a home either(3). How can we expect to maximize adherence if the client needs two weeks to learn the exercise correctly? For many of us, most of our clients are not pitchers trying to return to the mound, or hitters trying to get back to the volleyball court; they might just want to be able to reach overhead to put the dishes away. Keep in mind prior function and prior history of exercise as it relates to the complexity of the program you're prescribing exercise (4).
An Example of K.I.S.S.:
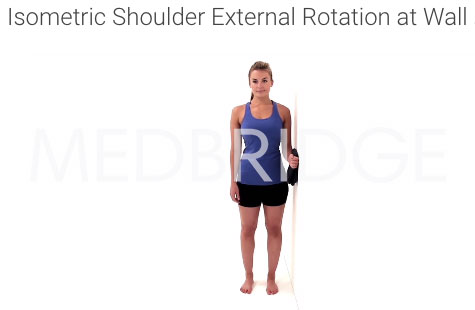
Anybody ever used this isometric exercise? Yeah... me too... many times.
The patient holds his/her elbow at his side taking one large step sideways and back to create and shoulder external rotation isometric. This is often performed in four directions, creating moving isometrics for flexion, extension, IR, and ER.
Compare it to the good ol' isometric vs the wall
The wall isometric isn't as "functional" as the reactive or stepping isometric, but does that make it worse? I used to prescribe the stepping isometric to every shoulder patient, that wasn't ready for isotonics, but now I only occasionally do. Why? Barriers to adherence limit this exercise:
It requires equipment that you have to provide or the patient has to buy
The equipment must be set up each time and available
If the elbow is tucked too tightly to the side of the body, load through the shoulder is mitigated
Steeper learning curve and reduced self efficacy (3)
Now I go with the standard isometric. The only equipment needed for adherence is a wall, and let's face it, most people a one "lying around"...
I never thought I'd be thinking about my eccentric, freshman biology teacher on a daily basis... Keep It Simple Stupid
References
1. Henry, Kristin D., Cherie Rosemond, and Lynn B. Eckert. "Effect of number of home exercises on compliance and performance in adults over 65 years of age." Physical Therapy 79.3 (1999): 270-277.
2. Littlewood, Chris, et al. "A self-managed single exercise programme versus usual physiotherapy treatment for rotator cuff tendinopathy: A randomised controlled trial (the SELF study)."Clinical rehabilitation (2015): 0269215515593784.
3. McLean, Sionnadh Mairi, et al. "Interventions for enhancing adherence with physiotherapy: a systematic review." Manual therapy 15.6 (2010): 514-521.
4. Der Ananian, Cheryl, et al. "Factors associated with exercise participation in adults with arthritis." J Aging Phys Act 16.2 (2008): 125-143.
Images:
Flickr Via Ben Russel "Teacher"
Thank you MedBridge for permitting use of the isometric images.
** This information is not intended to replace the advice of a physician/ physical therapist. Andy Parsons, PT, DPT disclaims any liability for the decisions you make based on this information.